Branch Retinal Vein Occlusion
Veins are responsible for returning blood to the heart. Smaller venules ultimately drain to the central retinal vein which carries blood from the eye. These smaller venules share a connective tissue sheath with arterioles. Arterial hypertrophy (enlargement) may occur due to hypertension (high blood pressure) or other medical conditions and compress these venules. When this hypertrophy occurs, venous stasis may lead to the occlusion (blockage) of the vein.
This venous stasis effectively causes the blood to be “backed up” similar to a blocked pipe. This also leads to ischemia of retinal tissue (decreased tissue oxygenation) and loss of capillary endothelial cells.
Patient symptoms include decreased vision, blurred vision, visual field deficit, and metamorphopsia (distortion). Some cases may be asymptomatic.
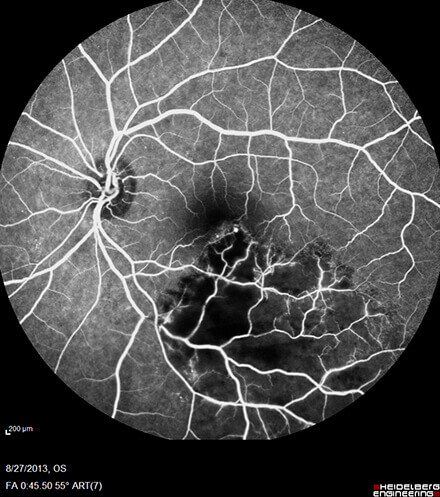
Common exam findings include intraretinal hemorrhages, cotton wool spots, and tortuous veins in the distribution of the branch retinal vein occlusion.
Common risk factors for this condition include glaucoma, hypertension, and obesity.
Central Florida Retina offers retinal angiography and optical coherence tomography which are critical tools in diagnosing branch retinal vein occlusion and following response to treatment.
This condition without treatment may advance to develop macular edema (swelling of the retina) and neovascularization (growth of abnormal blood vessels).
Treatments exist for branch retinal vein occlusion. Most commonly this may be treated with injections of medication into the eye. In the presence of neovascularization, treatments with panretinal photocoagulation (laser) may also be needed.
The surgeons at Central Florida Retina are fellowship trained retina specialists practicing the latest treatments for branch retinal vein occlusion. Should you be experiencing any of these symptoms or would like to request a consultation, please contact (800) 255-7188.



